It is important that we eliminate all misconceptions about excoriation disorder (aka, dermatillomania) and spread the word before these common myths become attached to this condition. Many of us have already heard several of the falsehoods listed below, so we need to make sure that these thoughts don’t become accepted views on what dermatillomania is or how it affects us.
1. MYTH: Skin pickers can stop at any time.
TRUTH: If this were true, we would have already stopped because it causes emotional distress having to deal with the aftermath of marks on our bodies.
Our brains are activated by a reward system that reduces anxiety once we get a “good pick”, which can make us feel accomplished thus enforcing the behavior. By the time we get a diagnosis, we will already have the behavior ingrained in our daily rituals, making it much more difficult to reverse.
We pick at our skin to reduce anxiety but then become anxious because of the visible marks left behind, which heightens our anxiety, causing us to engage in the behavior again as a way to reduce that anxiety, creating a vicious cycle.
2. MYTH: All skin pickers have an underlying skin condition causing the need to pick.
TRUTH: While many people start picking at their skin due to skin disorders (ie. acne, eczema), not all have one to start with.
Having one can trigger the onset of dermatillomania, but many of us have started with picking at perceived flaws such as multiple pimples/ blackheads causing the compulsive behavior.
3. MYTH: Picking at your skin is self-harm.
TRUTH: Some people with dermatillomania engage in other self-harming behaviors, but it’s not connected to the disorder nor is there a direct correlation between the two.
A person who intentionally self-harms does so to feel the physical pain, which releases endorphins making them feel better. The pain can be a distraction to not have to cope with emotional turmoil. Skin pickers can enter a “trance-like state”, causing them to dissociate from the physical pain or not be aware that they’re engaging with the behavior.
4. MYTH: Everybody pops some zits, which means that we all have a bit of dermatillomania.
TRUTH: Dermatillomania isn’t as simple as popping a few pimples. There is an obsessive nature behind the urge, which is why excoriation disorder is officially classified under obsessive-compulsive and related disorders.
There’s a compulsive nature behind chronic skin picking; a need to ‘search’, subconscious act while watching TV, or even something you do while asleep. Skin picking becomes a disorder when you are unable to stop after repeated attempts and it affects day-to-day life.
5. MYTH: Compulsive skin pickers do it because they hate themselves.
TRUTH: Many people with dermatillomania have low self-esteem, but pick their skin for anxiety relief or for sensory stimulation.
Body-images arise or are exasperated by this disorder because we feel alone, can’t control our urges, and blame ourselves; it can also make skin pickers feel judged and misunderstood, which prevents us from feeling accepted. The stigma of the disorder and judgments about the condition of our skin fuels feelings of isolation and mistrust in others.
6. MYTH: People who pick at their skin do it for attention.
TRUTH: Quite the opposite, actually. We spend much of our time trying to cover up the damage we inflict with makeup or clothing so that we can face the world without anyone noticing our scars.
Many of us are ashamed of the marks on our skin not just because the action that caused it is at is from our hands. We try to hide the fact that we have this disorder because it isn’t well-known to the public and the stereotypes attached to it are damaging.
7. MYTH: People who pick their skin are under the influence of narcotics.
TRUTH: The fourth criteria in the DSM-5 for an excoriation disorder diagnosis states, “The symptoms are not caused by a substance or medical, or dermatological condition“.
Methamphetamine is a stimulant that can result in skin picking from hallucinations of something under the skin, which falls under an amphetamine psychosis. It is also a stimulant that increases focus and speeds up thought processes, which can also induce obsessive behavior. Once the drug is removed from the body, the person’s behavior is likely to disappear if it was the source of the picking.
8. MYTH: Skin pickers see things on or under their skin that aren’t there; they are experiencing a psychosis.

TRUTH: Although there may be skin pickers who experience psychoses, there is no correlation between compulsive skin picking or any delusional disorder, except one.
Delusional parasitosis consists of a separate pathology than excoriation disorder. The behavior often discontinues once the psychosis is treated.
Other common co-morbid disorders often found dermatillomania are obsessive-compulsive disorder (OCD), body dysmorphic disorder (BDD), anxiety disorders, trichotillomania or other BFRBs, depression, and personality disorders.
9. MYTH: If Dermatillomania was a real disorder, it would have been recognized before the DSM-5 release.
TRUTH: Trichotillomania (hair pulling disorder) was added to the DSM III-R while skin picking remained a symptom of other disorders.
It was considered to be self-injurious but wasn’t further explored as a stand-alone disorder until May of 2013 with the release of the DSM-5 under the name excoriation disorder. Dermatillomania can disrupt a person’s life so greatly that by the time people seek treatment, it has already created problems in other areas of functioning.
10. MYTH: Picking at your skin is just a bad habit.
TRUTH: While the behavior of skin picking can be considered habitual in nature, dumbing it down to “habit” is hurtful.
The phrase “bad habit” can be attributed to chronic annoyances such as cutting toenails without throwing away the clippings, or never wiping crumbs off of a counter after fixing a sandwich. It is more accurate, and less dismissive, to categorize excoriation disorder as a compulsive mental health condition.
11. MYTH: Skin picking isn’t a serious issue; it’s superficial.
TRUTH: The act of popping a few zits is harmless, but excoriation disorder IS a serious issue that affects all facets of life. Social and physical isolation, suicidal ideations, scarring, embarrassment, a lack of control that can make daily functioning difficult.
Physically, skin pickers are more prone to infections, including antibiotic-resistant types like MRSA. The dissociative trance-like state can cause people to accidentally tear into muscle or veins/ arteries that need immediate medical attention.
It may seem superficial to many, but when you are scarred by your own hands, the guilt can be embarrassing and shameful enough to consume a person.
12. MYTH: There is no treatment for dermatillomania.
TRUTH: Here is the good news- there are treatments for this disorder and recovery IS possible. While dermatillomania is highly resistant to treatment, there are science-based methods that are proven to help.
The most common treatments are cognitive behavioral therapy (CBT), which includes habit reversal therapy and stimulus control and/ or SSRI medication, along with Acceptance-Commitment Therapy (ACT). Barriers are effective in preventing skin pickers from engaging in the behavior, or in helping to notice that they are, while fiddle toys can keep anxious hands busy.
Research on the supplement called N-Acetyl Cysteine, which increases levels of gluthione in the body, shows evidence that it can reduce the urges of hair pulling when taken in higher dosages. It has not yet been looked into for long term use past three months, so it isn’t an approved method but shows promise for people with BFRB’s.
Share this article to further help make this disorder known so all skin pickers can have access to qualified treatment providers and educate the world about a little-known disorder that affects up to 5% of the population.
Check out the documentary Scars of Shame and Angela’s memoir FOREVER MARKED: A Dermatillomania Diary. Learn about her upcoming recovery book EMBRACING DERMATILLOMANIA: Through Pain & Recovery. Follow Angela on Facebook, Twitter, and Instagram.
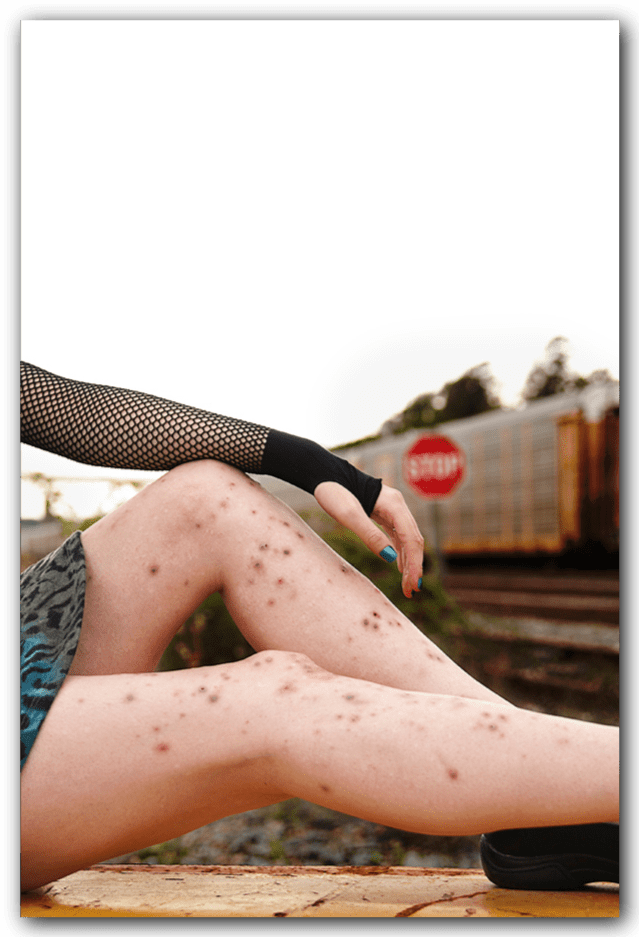
(Top left)
PHOTO: © Gillian Drake 2013
MODEL: Angela Hartlin
